Discover the multitude of processes and strategies involved in guaranteeing top-notch data quality in healthcare. Delve into the significance of data quality in the healthcare sector by exploring the valuable insights provided in this article.
Data quality management plays a crucial role in all organisations that engage in data sharing, analysis, or management. This importance is particularly evident in healthcare providers who deal with patients' medical records on a daily basis. Given the sensitivity of such data, strict regulations and protective measures are necessary.
To fully grasp the significance of healthcare data quality, healthcare providers must first comprehend the consequences of accessing this data and its impact on individuals. In order to access this data, healthcare providers must adhere to stringent rules and regulations. However, being aware of these regulations is not the sole requirement.
It is essential for organisations to recognise that obtaining a patient's medical information, including reports and records, has implications both for the individual and the treatment they receive. For example, let's consider an Australian healthcare provider, such as the Royal Melbourne Hospital. When accessing a patient's medical records, they must ensure the accuracy and completeness of the data. This means verifying the patient's personal details, medical history, allergies, and prescribed medications. Any errors or omissions in the data could lead to adverse events, such as prescribing the wrong medication or overlooking critical information during diagnosis.
By prioritising data quality and complying with regulations specific to Australia, such as the Australian Privacy Principles (APP) and the My Health Records Act, healthcare providers can safeguard sensitive information and simultaneously enhance patient outcomes. For instance, let's say a general practitioner in Sydney wants to share a patient's medical information with a specialist at a different clinic. To ensure data quality and protect patient privacy, the healthcare provider would need to obtain the patient's explicit consent and follow the guidelines set by the Australian Digital Health Agency for secure data sharing.
In addition to regulatory compliance, healthcare providers in Australia can also leverage data quality management to improve healthcare delivery. By maintaining accurate and reliable data, healthcare organisations can identify patterns and trends in patient outcomes, leading to evidence-based decision-making and better treatment plans. For instance, a hospital in Brisbane might use data analytics to examine the success rates of different surgical procedures and identify areas for improvement. This can ultimately result in enhanced patient care and improved overall healthcare outcomes.
In conclusion, healthcare data quality is of paramount importance in Australian healthcare. By understanding the implications of accessing and managing patient data, complying with regulations like the APP and the My Health Records Act, and leveraging data for evidence-based decision-making, healthcare providers can protect sensitive information, improve patient outcomes, and ultimately contribute to a more efficient and effective healthcare system in Australia.
Why is Data Quality Important in Healthcare Information Systems? Let's explore
The healthcare industry has undergone significant transformation due to technological advancements. The advent of software like Electronic Health Records (EHRs) has facilitated easier access to patients' medical data and histories. The seamless transfer of patient data brings numerous benefits, including optimised patient care through accurate data and a comprehensive patient overview.
However, to fully leverage these technological advancements, organisations must exercise caution regarding operational and administrative issues that may arise. Not all organisations are capable of managing high-quality data, which is crucial for reaping the benefits of these advancements.
Understanding the significance of data quality in healthcare involves recognising the fundamental principles of data, their value, and the potential challenges associated with data.
So, what exactly is data quality management?
While sharing patient information offers advantages, the sensitive nature of this data necessitates strict adherence to regulations by leading healthcare IT companies. Data quality management shares similarities with quality control. It involves the utilisation of technology, tools, and procedures to verify the sources of acquired data, thereby ensuring its integrity. The primary focus is to safeguard customers, or in this case, patients, by verifying information, integrating reliable sources, and transmitting data to trustworthy recipients. You can check more here.
Data quality in healthcare refers to the accuracy, completeness, consistency, timeliness, and relevancy of healthcare data. It is crucial to ensure that the data used in healthcare systems, electronic health records (EHRs), research studies, and analytics is reliable and trustworthy. High-quality data is essential for making informed clinical decisions, conducting meaningful research, and improving patient outcomes.
Here are some key aspects of data quality in healthcare:
- Accuracy: Data should be free from errors, discrepancies, or mistakes. It should reflect the correct information about patients, diagnoses, treatments, and other relevant healthcare details.
- Completeness: Data should be comprehensive and include all the necessary information required for a specific purpose. In healthcare, this may include patient demographics, medical history, laboratory results, medications, and treatment plans.
- Consistency: Data should be consistent across different sources and systems. It means that the same information should be recorded and represented in a standardised manner to avoid confusion or conflicting interpretations.
- Timeliness: Data should be up to date and recorded in a timely manner. It is crucial for healthcare providers to have access to the most recent patient information for accurate diagnosis, treatment, and care coordination.
- Relevancy: Data should be relevant to the specific purpose for which it is being used. Irrelevant or outdated data can lead to incorrect conclusions and potentially impact patient care.
- Data Privacy and Security: Implementing stringent measures to protect patient privacy and secure healthcare data. Adhering to relevant privacy regulations and guidelines, such as HIPAA in the United States or the Australian Privacy Principles in Australia.
- Data Integrity: Maintaining the accuracy, consistency, and reliability of healthcare data throughout its lifecycle. Implementing data validation checks and mechanisms to detect and prevent data corruption or tampering.
- Data Interoperability: Ensuring seamless exchange and integration of healthcare data across different systems, organisations, and platforms. Implementing interoperability standards, such as HL7 or FHIR, to enable effective data sharing and communication.
- Data Governance: Establishing clear roles, responsibilities, and processes for managing healthcare data. Defining data stewardship, data ownership, and accountability frameworks to ensure data quality and compliance.
- Data Auditability: Enabling traceability and audit trails to track the origin, changes, and access to healthcare data. Implementing logging mechanisms and data versioning to support data integrity and regulatory compliance.
- Data Quality Monitoring and Improvement: Regularly monitoring and assessing data quality metrics and indicators. Implementing data quality improvement initiatives, such as data cleansing, standardisation, and training programs, to continuously enhance data quality.
Ensuring data quality in healthcare involves various processes and strategies, such as data validation, data governance, data cleansing, and regular audits. It also requires adherence to data standards and best practices, as well as the use of advanced technologies and tools to monitor and improve data quality over time.
By maintaining high data quality standards, healthcare organisations can enhance clinical decision-making, optimise resource allocation, support population health management, enable accurate research studies, and improve patient safety and outcomes.
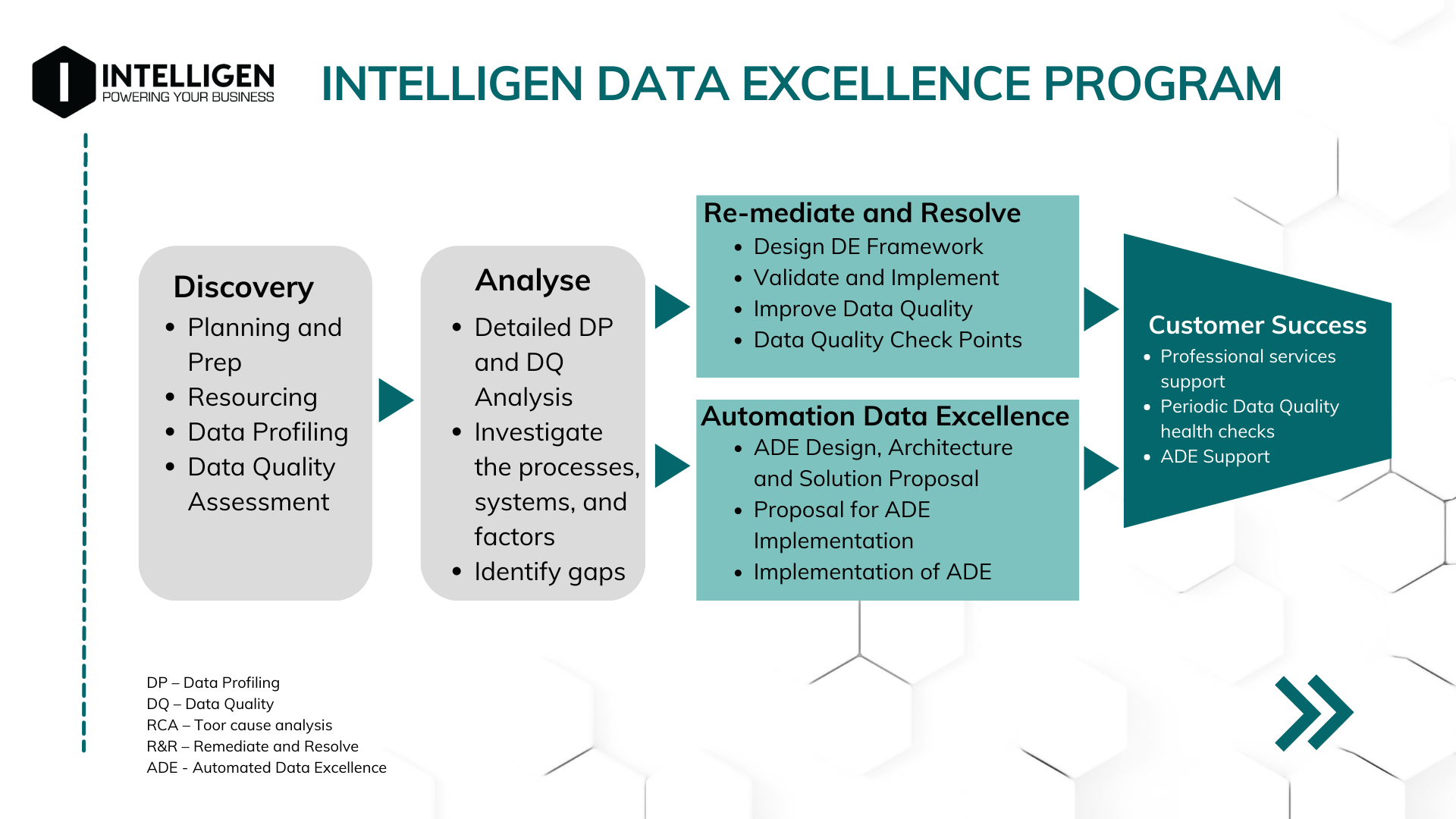
Just like the needed quality data in healthcare, our team of dedicated experts is ready to collaborate, strategise, and tailor powerful solutions to your unique business needs to achieve it. Get started and contact us today to find out more about our IDEP! 📞
These Posts are Suggested For You






